October 28, 2013
by Monica Mollica
Over the past decade, interest in anti-aging treatments and interventions aimed at promoting health, vitality and youthfulness over the life course into old age, has risen exponentially. The popularity and rise of anti-aging interventions has been fueled by the aging baby-boomer generation and the great dissatisfaction surrounding the current medical system in the US and many other Western nations.
Are you frustrated with today’s big-pharma dictated assembly line medicine with doctors who only spend 7 minutes per visit with their patients? Are you against the routine “have a symptom – take a pill” medical system mantra that is so pervasive in modern medicine? Then anti-aging medicine, a medical specialty developed and led by The American Academy of Anti-Aging Medicine (A4M) is for you.
The current medical system – background to the status quo
An editorial from the journal Clinical Interventions In Aging eloquently outlines the emergence of the current medical system status quo (1):
“Prior to the discovery of penicillin and production of antibiotics, extrinsic disease was the greatest threat to achieving maximum life potential (longevity). That single event increased life-span several decades for the majority of people living in first world nations. However, protection against lethal infection provided by antibiotics exposed older humans to a wide variety of life-threatening diseases resulting from disintegration of internal order during senescence. These intrinsic diseases including diabetes, stroke, heart attack, cancer, and a multitude of others, resulted in creation of medical
subspecialties. Although each specialty focused upon different organs and systems, they all administered treatment in response to disease. In other words, the operative model for modern medicine which deals with intrinsic disease is the same as that which was used for extrinsic disease, i.e., a disease occurs and then it is treated.
However, unlike therapy for infection which generally cures disease, treatment of intrinsic diseases only provides symptomatic relief, rarely affecting the underlying causes. Also, because it targets specific symptoms, this approach treats the disease condition as an isolated entity, independent of other bodily functions. Thus, the cardiologist, neurologist, allergist, and dermatologist focus their attentions only upon problems occurring within the system(s) limited by their training. Accordingly, they prescribe drugs that were created to specifically suppress or relieve symptoms directly related to the problem(s).
Despite the fact that this approach rarely provides a cure, it is effective in extending life, if not necessarily its quality, because many of the symptoms of intrinsic disease such as extremely high blood pressure, severe hyperglycemia, or profound breathing difficulties can lead to fatal complications.
The pharmaceutical industry fits well within the disease model for medical practice. This is because advances in cellular biology and biochemistry allow medicinal chemists to design compounds capable of modulating receptor, enzyme, and other molecular functions that block or attenuate the symptoms of underlying disease. Generally these effects are accompanied by secondary and unintended metabolic consequences. However, if the net result of administering the compound is to relieve primary symptoms then a simple and measurable indicator of efficacy has been achieved and a new drug is born. In other words, the pharmaceutical industry embraces the disease-oriented approach to medical practice because it provides a simple and unambiguous measure of efficacy for their products.
With continuing research into the consequences of aging, it is becoming apparent that medical practice must evolve from this disease-oriented model to one that is health-directed so as to ensure quality of life with longevity. In this alternative approach, patient health and vitality is prolonged and onset of intrinsic disease(s) is delayed or even prevented well into old age.
Although this approach is currently being employed by practitioners around the world, it is widely opposed by many in the traditional medical community and especially by the pharmaceutical industry. One reason for this reluctance is that a health-directed approach to medicine blurs the line between specialties since it requires consideration of the entire body and its interrelated functions, rather than single systems in isolation. This requirement tends to diminish a specialist’s expertise and thus is unacceptable to some. As a result, it is not surprising that medical practitioners who are committed to their individual specialty are not willing to accept change.
Another reason is that effective interventions that delay or prevent consequences of aging are not as easily demonstrated, because rather than simply reducing the intensity of preexisting symptoms (as is required in the disease-oriented treatments), proof for health-oriented interventions requires that efficacy be demonstrated by the absence or delay in onset of symptoms. This type of proof requires advanced and sensitive measurement technologies and need long-term studies.”
Thus, current medicine is effective in preventing death from age-related diseases without curing the diseases or delaying their onset. While preventing deaths, this disease-oriented medical approach increases in the number of people with age-related diseases. In addition, each disease of aging is now treated separately, which is costly and can lead to unintended and unavoidable adverse effects. For example, chemotherapy, used for cancer treatment, has a negative impact on normal tissues and organs. And insulin, which is used for diabetes, has pro-aging effects (2) and may accelerate some pathologies, such as cancer (3, 4).
Proof that the current disease-oriented medical system isn’t working
Recent reports show that the disease oriented traditional medical approach isn’t helping us:
* 7 out of 10 deaths among Americans each year are caused by chronic lifestyle-related diseases (5). By 2020, their contribution is expected to rise to 73% of all deaths globally (5, 6).
* Cardiovascular diseases (CVD) remain the leading cause of morbidity and mortality in modern societies, followed by cancer (7, 8). In 2009, cardiovascular diseases accounted for 32.3% of all deaths, or 1 of every 3 deaths in the United States (8).
* In 2009, 34% of deaths attributable to cardiovascular diseases occurred before the age of 75 years, which is well before the average current life expectancy of 78.5 years (8).
* In 2005, 133 million Americans had at least one chronic illness (9).
* Overweight / Obesity has become a major health concern. Among Americans age 20 and older, 154.7 million are overweight or obese (8). The current US population is 316.7 million (10); thus close to 49%, or almost 1 out of every 2 adults, are overweight or obese.
* In 2010, more than one third of children and adolescents were overweight or obese (11).
* Obesity is associated with 20% higher all-cause mortality in adults (12), and between 1990 and 2010, DALY (disability-adjusted life-years, which is the sum of years of life lost due to premature mortality and years lived with disability) related to elevated BMI, independent of diet composition, increased by 45% (13). If past obesity trends continue unchecked, the negative effects on the health of the U.S. population will increasingly outweigh the positive effects gained from declining smoking rates. Failure to address continued increases in obesity could result in an erosion of the pattern of steady gains in health observed since early in the 20th century (14).
* Obesity in childhood and adolescence often tracks into adulthood, and elevates obesity-induced health risks later in life. For type-2 diabetes, obese adults who were also overweight or obese in childhood and adolescence have 12.6 higher odds, than for those who were obese in adulthood only (15). A similar trend is seen for cardiovascular risk in later life (15, 16).
* 33 % of US adults (78 million) over 20 years of age have high blood pressure (8). Among these, almost 20 % aren’t aware of their condition (8).
* High blood pressure is a major and most common risk factor for developing cardiovascular disease and mortality (17). The mortality risk doubles for every 20-mmHg increase in systolic blood pressure above the threshold of 115mmHg and for every 10-mmHg increase above the diastolic blood pressure threshold of 75mmHg (18).
* In 2010, an estimated 19.7 million Americans had diagnosed diabetes, representing 8.3% of the adult population. An additional 8.2 million had undiagnosed diabetes, and 38.2% had pre-diabetes, with elevated fasting glucose levels (8). The prevalence of diabetes is increasing dramatically, in parallel with the increases in prevalence of overweight and obesity.
* On the basis of NHANES 2003–2006 data, the age-adjusted prevalence of metabolic syndrome, a cluster of major cardiovascular risk factors related to overweight/obesity and insulin resistance, is approximately 34% (35.1% among men and 32.6% among women) (8).
* The United States spends significantly more on health care than any other nation. In 2006, our health care expenditure was over $7,000 per person (19), more than twice the average of 29 other developed countries (20). We also have one of the fastest growth rates in health spending, tripling our expenditures since 1990 (19). Yet the average life expectancy in the United States is far below many other nations that spend less on health care each year.
* An increasing percentage of health care dollars spent in the U.S. are spent on people with chronic conditions. In 2004, the care given to people with chronic conditions accounted for 85 % of all of health care spending (21).
* In 2000, the annual direct cost of physical inactivity in the USA was estimated as $76.6 billion (22).
* The total number of inpatient cardiovascular operations and procedures increased 28% between 2000 and 2010 (8).
* The total direct and indirect cost of CVD and stroke in the United States for 2009 was $312.6 billion. By comparison, in 2008, the estimated cost of all cancer and benign neoplasms was $228 billion. CVD costs more than any other diagnostic group (8).
* In treating patients with chronic conditions, 66% of physicians believe their training did not adequately prepare them to educate patients with chronic conditions, and provide effective nutritional guidance (23).
* The largest number of people with chronic conditions is of working age and is privately insured: 78 million people with chronic conditions have private insurance coverage and their care accounts for about 73 % of private insurance spending. Almost all Medicare dollars and about 80% of Medicaid spending is for people with chronic conditions (21).
What are the causes behind the surge of chronic age-related diseases?
The risk factors for these chronic diseases are mainly caused by unhealthy lifestyles (24). Four modifiable health risk behaviors – lack of physical activity, poor nutrition, tobacco use, and excessive alcohol consumption – are responsible for much of the illness, suffering, and early death related to chronic diseases. Due to the importance of physical inactivity for morbidity and mortality, it has recently been suggested that physical inactivity per se should be regarded as a disease (25).
Stats related to unhealthy lifestyles:
* People consistently overestimate their own health behavior; almost 90% rate themselves as healthy. The reality is that 9 out of 10 have at least one risk factor for heart disease and stroke (26).
* Among young adults aged 18-39 years, only 20% meet low risk criteria, and almost 60% have high levels of at least one risk factor (27). In young adult and middle-aged populations, aged 18 to 59 years, only 5-10% have a low health risk status (28).
* Risk factor measurements in children, obtained at or after 9 years of age, are predictive of subclinical atherosclerosis and cardiovascular disease risk in adulthood (29). As children are not screened for health risks to the same extent as adults, this might contribute to an increased disease burden in the coming decades when today’s kids are grownups.
* Today very few Americans are at low risk for heart disease. Approximately 78% of adults aged 20-80 years alive today in the United States are candidates for at least one prevention activity (30). Over 55% of young adults have at least one cardiovascular disease risk factor, and over 37% reported having two or more (31).
* If everyone received the prevention activities for which they are eligible, heart attacks and strokes would be reduced by 63% and 31%, respectively (30). Of the specific prevention activities, the greatest benefits to the US population come from controlling pre-diabetes, weight reduction in obese individuals, lowering blood pressure, and improving blood lipids (30).
* Lack of regular exercise has been estimated to account for 23% of U.S. deaths, with these deaths being attributable to nine chronic diseases (32).
* Poor diet and physical inactivity were the second leading cause of preventable deaths from 1980–2002 (33).
* Data very strongly support an inverse association between lifetime physical activity and all-cause mortality, with lifetime inactive individuals having over 30% higher risk of dying compared with lifetime active individuals (34).
* Majority of adults (81.6%) and adolescents (81.8%) do not get the recommended amount of physical activity (150 min/week) (35), and 23% report no leisure-time physical activity at all in the preceding month (36).
*32 percent of U.S. adults engage in no aerobic leisure-time physical activity (8).
* Only 1-3 % of adults attain at least 30 min moderate-to-vigorous physical activity per day from three or more bouts of at least 10 min (37, 38).
* Objective evaluations show that U.S. adults an average only achieve 45 minutes/week (6 min/day) of moderate physical activity and only 18 minutes/week (2.5 min/day) of vigorous physical activity (39).
* With regard to vigorous physical activity, 28% of men and 16% of women achieve 75 min/week and 13% and 7.0% achieve 20 min/day on 3 days/week (40).
*A recent study shows that among people who do meet the physical activity guidelines, only 34.9% of men and 21.6% of women attain an average physical activity level (PAL) of 1.75, the threshold for preventing weight gain (40). To increase overall physical activity levels, a high level of physical activity throughout the day would be required for most people. This explains why individuals who accumulate 30 min/day of moderate-to-vigorous physical activity but are otherwise sedentary during the day, may meet the guidelines for cardiovascular health, without achieving the minimum levels to avoid excessive weight gain (40).
* In 2007, less than 22% of high school students (41) and only 24% of adults (42) reported eating 5 or more servings of fruits and vegetables per day.
* A low intake of fish oil/fatty fish (less than 62 mg/day of EPA and DHA) compared to a higher intake of over 250 62 mg/day of EPA and DHA, more than doubles the risk for heart disease (43).
* Data from the National Health and Nutrition Examination Survey (NHANES) indicate that between 1971 and 2004, average total energy consumption among US adults increased by 22% in women (from 1542 to 1886 kcal/d) and by 10% in men (from 2450 to 2693 kcal/d) (8).
* The increases in calories consumed are attributable primarily to greater carbohydrate intake, in particular, of starches, refined grains, and sugars. Other specific changes related to increased caloric intake in the United States include larger portion sizes, greater food quantity and calories per meal, and increased consumption of sugar-sweetened beverages, snacks, commercially prepared (especially fast food) meals, and higher energy-density foods (8).
Impact of improved lifestyle habits
The importance of lifestyles for health promotion and anti-aging is underscored by the fact that although genetic factors and age (which are non-modifiable risk factors) are important in determining cardiovascular disease, modifiable risk factors are the major contributors to cardiovascular morbidity and mortality, and account for 90% of all heart attacks (44-47).
Examples of modifiable risk factors that have major consequences for health and determine how gracefully an individual will age, are abdominal obesity, abnormal blood lipoprotein profiles, diabetes, unhealthy food habits, and lack of regular physical activity.
Because a sedentary lifestyle accelerates the aging process (48-52), regular physical activity/exercise is a cornerstone in the anti-aging arsenal:
* 1 vigorous workout per week has been shown to be associated with a 39% reduction in mortality for men and 51% reduction in mortality for women (53).
* Moderate-intensity exercise for 15 min a day can reduce all-cause and all-cancer mortality and extended an individual’s lifespan for an average of 3 years (54). This minimum amount of exercise was found to be applicable to men and women of all ages, even those with cardiovascular diseases or lifestyle risks.
* For each minute increase in treadmill time on a maximal exercise test made 5 years apart, there was a corresponding 8% decrease in risk of mortality, regardless of baseline health status (55).
* Regular exercise and physical activity is associated with a reduced risk by as much as 60% of developing many common diseases, such as the metabolic syndrome, diabetes, cardiovascular diseases, breast cancer, colon cancer, prostate cancer, pancreatic cancer, high blood pressure, osteoporosis, Alzheimer’s, asthma and arthritis (56, 57).
* Regular vigorous exercising can postpone disability by 16 years (58).
* It has been estimated that inactive persons would gain up to almost 4 added years from age 50 by becoming active (59, 60).
* Minimal adherence to current physical activity guidelines, which yield an energy expenditure of about 1000 cal per week, is associated with an up to 30% reduction in risk of all-cause mortality (61). Further reductions in risk are observed at higher volumes of physical activity related energy expenditure (61).
* Reducing sitting time to 3 h/day or less is estimated to increase life expectancy in the US population by 2 years (62). Today, people in the US on average spend about 8 hours daily, i.e. half of their waking time, being sedentary (63).
* Among older adults, compared to those who were sedentary for 4 hours/day or more, those who were moderately (2–4 hours/day) and least sedentary (less than 2 hours/day) were 38% and 43% more likely to age successfully, respectively. Among middle-aged adults, those who were least sedentary were also 43% more likely to age successfully (64).
Food habits and nutrition is the other major lifestyle factor that can confer substantial health benefits and help stave off many chronic diseases (65-68):
* A non-calorie restricted Mediterranean diet supplemented with extra-virgin olive oil (33 fl oz per week) or 30 g raw nuts per day (15 g of walnuts, 7.5 g of hazelnuts, and 7.5 g of almonds), consumed for 5 years reduces the incidence of major cardiovascular events by 30% among persons at high cardiovascular risk (69). After 1 year, the same Mediterranean diet supplemented with 30 g raw nuts per day reduces waist circumference by 2 inches (5cm) (70).
* Compared to consuming less than 1 serving/wk of nuts, people consuming 3 servings/wk (about 25 g/day) or more, have a 39% reduced risk for obesity, 26% reduced risk for the metabolic syndrome, and 13% reduced risk for diabetes (71). Higher nut consumption was also associated with a 32% lower risk of abdominal obesity (71).
* Walnut consumption, 2 servings (60 g) per week or more compared with non-consumption or rare consumption, is associated with a 33% lower risk of type 2 diabetes (72).
* People with a high intake of flavonoids (which are health promoting substances found in fruits and vegetables), 360 mg/day, corresponding to 20 serving/week of fruits and 24 servings/wk of vegetables have been found to have a lower risk of fatal cardiovascular disease by 18%, compared to those with a low intake of 120 mg of flavonoids/day (73).
*High blood levels of omega-3 fatty acids (and by implication omega-3 fat intakes) are associated with 27% lower total mortality, especially from cardiovascular deaths (74). This mortality difference corresponds to 2.2 more years of remaining life after age 65 in people with higher versus lower omega-3 levels (74).
* Adhering to a healthy diet, characterized by high intakes of fruit, vegetables, fiber, fish/shellfish, and low intake of sugar, has been associated with a reduced incidence of cardiovascular (CV) events by 32% in and 27% in women (67).
* In a meta-analysis of over 300,000 American, Japanese, and Chinese middle-aged participants, higher dairy consumption (>3 servings/day versus <1 serving/day) was associated with a 15% reduced risk of type 2 diabetes (75). A dose-response analysis showed that the risk of type 2 diabetes could be reduced by 5% for each additional serving of total dairy products and by 10% for each additional serving of low-fat dairy products consumed (75).
* The combination of the main healthy lifestyle factors – maintaining a healthy weight, exercising regularly, eating healthy, and not smoking or abusing alcohol – seem to be associated with as much as an 80% reduction in the risk of developing the most common and deadly chronic diseases (76).
* Among individuals aged 70 to 90 years, adherence to a Mediterranean diet and healthy lifestyle with regular physical activity is associated with a more than 50% lower rate of all-causes and cause-specific mortality (77).
What are Americans most concerned about when getting old?
According to a poll conducted by ABC News/USA Today, the most prominent concerns about aging are (78):
* Losing one’s health 73%
* Losing ability to care for oneself 70%
* Losing mental abilities 69%
* Not being able to drive/travel on one’s own 59%
* Being a burden on one’s family 54%
* Winding up in a nursing home 52%
* Not being able to work or volunteer 49%
Amidst the epidemic of chronic diseases, it is not surprising that the top concern about aging include poor health, being unable to care for yourself and losing mental acuity. People are increasingly turning to anti-aging doctors for answers to these health concerns.
Insufficient clinical training in traditional medical school
The disease-based model of healthcare has significantly influenced medical school curricula (79). More medical students believe lifestyle changes are important when they begin medical school than when they finish (80). This shows the negative impact the current curricula have on the motivation of future healthcare providers regarding lifestyle behaviors (80-82).
The American Board of Medical Specialties lists 24 specialties and 121 subspecialties; integrating knowledge from these fields into a disease prevention/anti-aging curriculum would be overwhelming (83). Education on preventive medicine is widely considered inadequate, and there is little, if any, attention paid to health promotion or prescribing physical activity (84, 85). This was underscored by a study that investigated the views of leaders in academic medicine concerning the need for programs in preventive medicine and the prevailing barriers to program development (85). It was found that:
- 91% considered academic preventive medicine underdeveloped.
- 100% considered their own programs average or worse.
- 80% perceived a shortage of preventive medicine faculty.
- 60% considered preventive medicine research quality to be inadequate.
Identified barriers to development and advancement of preventive medicine included funding constraints, academic bias to biomedicine, inadequate quality of preventive medicine research and faculty, preferences for technologic care, and the organization of academic medical centers. It was concluded that overcoming these barriers would require a change in our understanding of the tremendous role of prevention for improving health across the lifespan (85).
Medical students acquire sparse knowledge about prevention, and they see this field as an unappealing career choice, in large part due to the sparse funding in the area compared to well established medical specialties (83, 86). The importance of including the subject of preventive medicine in medical degree programs has been internationally recognized and has led to a number of initiatives to improve the incorporation of prevention into routine healthcare (87). The most well-known organization dedicated to help implement preventive medicine into the medical system is The American Academy of Anti-Aging Medicine, a.k.a. A4M.
What is Anti-Aging Medicine?
Motivated by discouraging disease trends, and guided by scientific research advances in our understanding of the mechanisms and causes behind chronic age-related diseases, The American Academy of Anti-Aging Medicine (A4M) was developed.
Anti-aging medicine is a relatively new, but quickly growing, medical specialty founded and led by A4M, with the mission, as stated on their website www.AntiAgingAge.com/about/about-a4m:
“To advance technology and implement practices to detect, prevent, and treat aging related disease and to promote research into mechanisms and interventions to retard and optimize the human aging process.
The American Academy of Anti-Aging is also dedicated to educating physicians, scientists, and members of the public on biomedical sciences, breaking technologies, and anti-aging issues. The American Academy of Anti-Aging believes that the disabilities associated with normal aging are caused by physiological dysfunctions which in many cases can be prevented or improved by lifestyle and/or medical interventions. In this way, The American Academy of Anti-Aging Medicine posits that chronological age and biological age do not have to coincide, and that both the human lifespan and health span can be increased as people grow older chronologically.
The American Academy of Anti-Aging seeks to disseminate information about innovative science and research, as well as treatment modalities designed to prolong and improve the human lifespan.
Anti-Aging Medicine is based on the scientific principles of evidence based medicine. Although The American Academy of Anti-Aging disseminates information on many types of medical treatments, it does not promote or endorse any specific treatment nor does it sell or endorse any commercial product.”
Thus, the mission of The American Academy of Anti-Aging Medicine (A4M) is essentially to help people live healthier and happier for longer. By compressing morbidity that arises from chronic lifestyle related diseases, which currently account for the majority of both premature and late-life mortality, A4M makes the case that increasing healthspan will also increase life span and the years spent living in youthful vigor.
What distinguishes doctors who practice Anti-Aging Medicine under the guidance of A4M?
A4M emphasizes individualized care; this is evident from the first visit, with A4M board certified doctors reporting that they spend between two and five hours with new patients (88). A4M doctors are less concerned about assigning a disease label to a patient’s problems than they are about uncovering its causes and underlying processes. They see “the patient who has the disease” not “the disease of the patient”. In line with this, they take extensive lifestyle histories that include things traditional medicine often neglects, such as nutrition, exercise, sleep habits, supplements, stress etc.
Here are two insightful quotes from interviews with A4M doctors (88):
“We spend more time with our patients. We dig a little deeper. We’re looking at the whole person…. A lot of conventional doctors would say ‘Well it’s in range, you’re fine’. We look beyond the ‘normal’ ranges and look for the optimal ranges. So we’re kind of focused more on optimal health, versus just normal, and on treating the underlying cause instead of just matching a drug with the bug.”
“We look at the whole person, all of the disease processes put together and trying to find out what is the core reason and what are the causative factors, whereas in conventional medicine we all work in a silo. I mean the orthopedists do theirs, and somebody’s got a foot specialist and a hand specialist and an ear specialist, and right now current medicine is fragmental where doctors do their own thing. We try to put all those pieces of the puzzle together.”
This emphasis on “optimal health” instead of just “normal” is the reason anti-aging medicine doctors see themselves as being in the vanguard of medicine (88, 89). Their goal is to create optimal functioning, and not be satisfied when tests and functioning falls within “normal” ranges defined statistically. Anti-aging medicine doctors also prefer to define “normal” ranges based on the individual patient in question, in order to improve the patient’s health and achieve an optimal state of being that is individually defined. They see their patients as unique individuals and not as the mean in a graph of statistical dots.
Anti-aging medicine doctors reject the traditional “disease model” of medicine – which that focuses on
standardized measures and tests and on uniform diagnoses – in favor of strategies that allow them to gain a deeper perspective on why patients have particular symptoms. The modes of treatment they choose are preventive ones. For example, if a patient presents with blood sugar levels in the upper end of the “normal” range, the anti-aging medicine doctor will educate the patient on the importance of exercise and proper nutrition, instead of saying “your level is within range, you’re fine” and wait for diabetes to develop, at which point they simply prescribe a medication.
This is illustrated by another insightful quote from an A4M doctor (88):
“There is minimal emphasis on prevention in medical school. … no one cares about it and typical doctors don’t know much about it. They are a lot more interested in learning how to do a bypass surgery than they are in what the optimal dose of calcium is to prevent osteoporosis, how exercise can improve cardiovascular system etc, and things along those lines.”
Primary Prevention – the future of medicine and healthspan extension
As outlined above, A4M certified doctors embrace the power of primary prevention, e.g. strategies that prevent the development of diseases in the first place. Primary prevention keeps the disease process from becoming established by eliminating causes of disease and/or by increasing resistance to disease (91, 92). Anti-aging doctors fill a void in wellness-oriented preventive healthcare that is sought by an increasingly greater segment of the population as it ages (93).
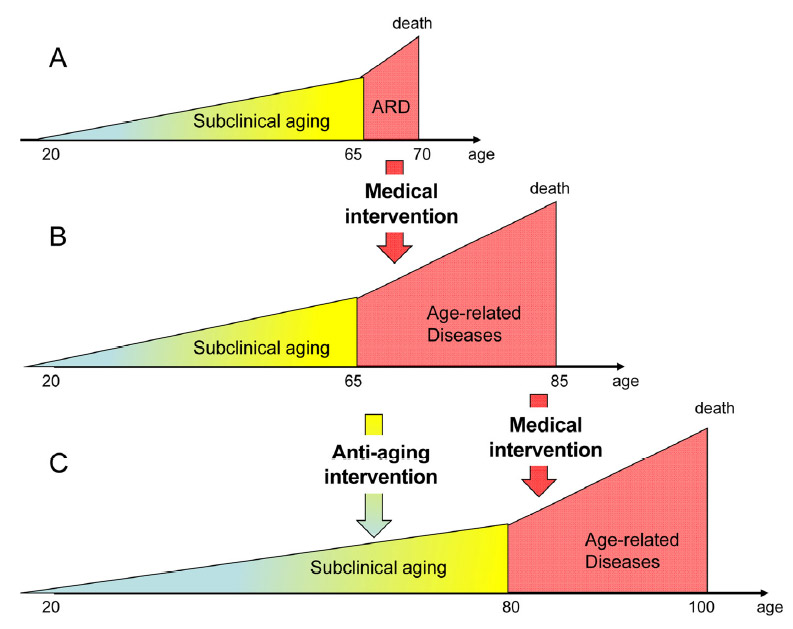
Figure 1 below nicely illustrate the essence of anti-aging medicine; from longer life span to longer health span (and life span) (94).
From A to B: Standard medicine increases lifespan by preventing death from age‐related diseases. It simultaneously increases a number of old people suffering from age‐related diseases.
From B to C: Anti‐aging interventions will slow down processes that contribute to physiological declines associated with chronological aging, and delay the onset of age‐related diseases.
With progress in preventive and anti-aging medicine, and in helping people make lifestyle changes, the red area in the figure “age-related diseases” will become an even smaller part of the total lifespan due to compression of morbidity and consequent increases in healthspan (92, 95-98). This is illustrated in figure 2 (92):
Scenarios for future morbidity. Black areas represent cumulative morbidity.
(1) Present morbidity
(2) Life extension; a future where both life expectancy and morbidity are both increased
(3) Compression of Morbidity; a future where onset of morbidity is delayed, and lifespan in increased, resulting in Compression of Morbidity and an increase in healthspan.
Proof that compression of morbidity is possible in reality comes from several studies of exceptional longevity in centenarians (people over 100 years old) (99-102). Super-centenarians (those over age 105) have proved to have had less lifetime cumulative morbidity than those dying at age 85 or 100 (99). This suggests that a healthy lifestyle that prevents onset of chronic diseases and morbidity can help everybody increase both their lifespan and healthspan.
Further proof that is it unhealthy lifestyles, and not the biological aging process, that cause impairments to physical performance that commonly start to manifest in middle age, comes from studies of master athletes (103, 104). For example, it has been found that 25% of the 65-69 year old runners were faster than 50% of the 20-54 year old runners (103). This survey also revealed that more than 25% of the 50-69 year-old runners had started their marathon training only in the past 5 years (103). Thus, performance losses in middle age are mainly due to a sedentary lifestyle, rather than biological aging. This shows that even at an advanced age non-athletes can achieve high levels of performance through regular training.
Researchers have suggested that centenarians and master athletes are ideal models for studying healthy/successful aging and search for clues that can help everybody age well (100-102, 105, 106). These populations show us that the aging process is modifiable, and that healthspan extension is a viable option for everybody to pursue via daily lifestyle choices.
Conclusion
In stark contrast to traditional medicine, which focuses on treatment of diseases and disturbed health (1, 90), the main objective of anti-aging medicine is health promotion and disease prevention, primarily through healthy lifestyles with regular exercise/physical activity and proper nutrition.
Anti-Aging Medicine is the fastest-growing medical specialty throughout the world. The specialty was originally developed by The American Academy of Anti-Aging Medicine (A4M), and is founded on the application of advanced scientific technologies for the early detection, prevention, treatment and reversal of age-related dysfunction, disorders and diseases. It is a health care model promoting innovative science and research to prolong the healthy lifespan in humans.
The term “anti-aging” relates to the application of advanced biomedical technologies focused on the early detection, prevention and treatment of aging-related disease. The goal of anti-aging is not to merely prolong the total years of an individual’s life, but to ensure that those years are enjoyed in a healthy, productive and vital state.
In the US, over 85% of our health care dollars go to treatment of chronic lifestyle induced diseases. These persistent conditions – the nation’s leading causes of death and disability – cause deaths that could have been prevented, lifelong disability, compromised quality of life, and burgeoning health care costs.
Guided by advances in health promotion and medical research, A4M encourages doctors to personalize treatments based on every patient’s unique circumstances, and not succumb to statistically driven medical decision making, which characterizes the current medical system.
A4M also encourages people to learn about their health status and risks factors. Asymptomatic diseases or risk factors for non-communicable diseases are extremely frequent among the general population (107). And most people are not sufficiently aware of their health risks to act up and change their lifestyle and take appropriate preventive measures (107). By becoming actively involved in improving ones health by making healthy lifestyle choices, everybody can take personal control over their health and aging destiny.
More information and valuable resources can be found on The American Academy of Anti-Aging Medicine website www.AntiAgingAge.com
About the Author:
————————————–

Monica Mollica has a Bachelor’s and Master’s degree in Nutrition from the University of Stockholm, Sweden, and is an ISSA Certified Personal Trainer. She works a dietary consultant, health journalist and writer for www.BrinkZone.com, and is also a web designer and videographer.
Monica has admired and been fascinated by muscular and sculptured strong athletic bodies since childhood, and discovered bodybuilding as an young teenager. Realizing the importance of nutrition for maximal results in the gym, she went for a BSc and MSc with a major in Nutrition at the University.
During her years at the University she was a regular contributor to the Swedish bodybuilding magazine BODY, and she has published the book (in Swedish) “Functional Foods for Health and Energy Balance”, and authored several book chapters in Swedish publications.
It was her insatiable thirst for knowledge and scientific research in the area of bodybuilding and health that brought her to the US. She has completed one semester at the PhD-program “Exercise, Nutrition and Preventive Health” at Baylor University Texas, at the department of Health Human Performance and Recreation, and worked as an ISSA certified personal trainer. Today, Monica is sharing her solid experience by doing dietary consultations and writing about topics related to health, fitness, bodybuilding, anti-aging and longevity.
References:
1. Walker RF. Challenges facing age-management/longevity medicine. Clinical interventions in aging. 2007;2(2):175-177.
2. Bartke A. Insulin and aging. Cell Cycle. 2008;7(21):3338-3343.
3. Bowker SL, Majumdar SR, Veugelers P, et al. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes care. 2006;29(2):254-258.
4. Hammarsten J, Hogstedt B. Hyperinsulinaemia: a prospective risk factor for lethal clinical prostate cancer. Eur J Cancer. 2005;41(18):2887-2895.
5. Kung HC, Hoyert DL, Xu JQ, et al. Deaths: final data for 2005. National Vital Statistics Reports Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf 2005.
6. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS medicine. 2006;3(11):e442.
7. Murphy SL, Xu JQ, Kochanek KD. Deaths: final data for 2010. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6208a8.htm 2010.
8. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6-e245.
9. Wu SY, Green A. Projection of chronic illness prevalence and cost inflation. RAND Health; Santa Monica, CA 2000.
10. Bureau USC. U.S. and World Population Clock. http://www.census.gov/popclock/ 2013.
11. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307(5):483-490.
12. Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA : the journal of the American Medical Association. 2013;309(1):71-82.
13. Murray CJ, Abraham J, Ali MK, et al. The State of US Health, 1990-2010: Burden of Diseases, Injuries, and Risk Factors. JAMA : the journal of the American Medical Association. 2013.
14. Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. The New England journal of medicine. 2009;361(23):2252-2260.
15. Park MH, Sovio U, Viner RM, et al. Overweight in childhood, adolescence and adulthood and cardiovascular risk in later life: pooled analysis of three british birth cohorts. PloS one. 2013;8(7):e70684.
16. Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond). 2011;35(7):891-898.
17. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
18. Vasan RS, Larson MG, Leip EP, et al. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358(9294):1682-1686.
19. Services CfMaM. National health expenditures aggregate, per capita amounts, percent distribution, and average annual percent growth, by source of funds: selected calendar years 1960–2007. Available from: http://www.cms.hhs.gov/NationalHealthExpendData/downloads/tables.pdf: Baltimore, MD 2008.
20. (OECD) TOfEC-oaD. Health at a Glance 2011 – OECD indicators. http://www.oecd.org/els/health-systems/49105858.pdf: Organisation for Economic Co-operation and Development, Paris. 2011.
21. Anderson G. Chronic conditions: making the case for ongoing care. . Baltimore, MD: John Hopkins University 2007.
22. Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics–2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25-146.
23. Ciemnecki AB, Diaz-Tena N, Fishtein J, et al. National Public Engagement Campaign on Chronic Illness – Physician Survey. Mathematica Policy Research, Inc. 2001.
24. WHO. The world health report 2002 – Reducing Risks, Promoting Healthy Life 2002. http://www.who.int/whr/2002/en/whr02_en.pdf 2002.
25. Weiler R, Stamatakis E. Physical activity in the UK: a unique crossroad? British journal of sports medicine. 2010;44(13):912-914.
26. Heart and Stroke Foundation. Report on Canadians’ Health. Denial is putting Canadians at high risk of cutting their lives short. . 2011.
27. Daviglus ML, Stamler J, Pirzada A, et al. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA : the journal of the American Medical Association. 2004;292(13):1588-1592.
28. Stamler J, Stamler R, Neaton JD, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA : the journal of the American Medical Association. 1999;282(21):2012-2018.
29. Juonala M, Magnussen CG, Venn A, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. 2010;122(24):2514-2520.
30. Kahn R, Robertson RM, Smith R, et al. The impact of prevention on reducing the burden of cardiovascular disease. Circulation. 2008;118(5):576-585.
31. Services UDoHaH. National Center for Health Statistics. Health, United States, 2010. CDC 2010.
32. Hahn RA, Teutsch SM, Rothenberg RB, et al. Excess deaths from nine chronic diseases in the United States, 1986. JAMA : the journal of the American Medical Association. 1990;264(20):2654-2659.
33. Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the United States, 2000. JAMA : the journal of the American Medical Association. 2004;291(10):1238-1245.
34. Services UDoHaH. Physical Activity Guidelines Advisory Committee Report. http://www.health.gov/paguidelines/Report/pdf/CommitteeReport.pdf 2008.
35. U.S. Department of Health and Human Services USDoA. Physical Activity Guidelines for Americans. Washington, DC: http://www.health.gov/paguidelines/guidelines/default.aspx 2008.
36. Centers for Disease Control and Prevention. Prevalence of self-reported physically active adults—United States, 2007. MMWR 2008;57:1297–1300. 2008.
37. Hagstromer M, Oja P, Sjostrom M. Physical activity and inactivity in an adult population assessed by accelerometry. Medicine and science in sports and exercise. 2007;39(9):1502-1508.
38. Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40(1):181-188.
39. Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. American journal of preventive medicine. 2011;40(4):454-461.
40. Scheers T, Philippaerts R, Lefevre J. Compliance with different physical activity recommendations and its association with socio-demographic characteristics using an objective measure. BMC public health. 2013;13:136.
41. Prevention CfDCa. Youth risk behavior surveillance—United States, 2007. MMWR 2008;57(SS-04):1–131: Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5704a1.htm 2008.
42. Prevention CfDCa. BRFSS prevalence and trends data. Atlanta, GA: Available from: http://apps.nccd.cdc.gov/brfss/page.asp?cat=AC&yr=2007&state=US#AC 2008.
43. Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS medicine. 2009;6(4):e1000058.
44. Dahlof B. Cardiovascular disease risk factors: epidemiology and risk assessment. The American journal of cardiology. 2010;105(1 Suppl):3A-9A.
45. Ignarro LJ, Balestrieri ML, Napoli C. Nutrition, physical activity, and cardiovascular disease: an update. Cardiovascular research. 2007;73(2):326-340.
46. Napoli C, Stanley WC, Ignarro LJ. Nutrition and cardiovascular disease: putting a pathogenic framework into focus. Cardiovascular research. 2007;73(2):253-256.
47. de Groot LC, Verheijden MW, de Henauw S, et al. Lifestyle, nutritional status, health, and mortality in elderly people across Europe: a review of the longitudinal results of the SENECA study. The journals of gerontology Series A, Biological sciences and medical sciences. 2004;59(12):1277-1284.
48. Booth FW, Hargreaves M. Understanding multi-organ pathology from insufficient exercise. J Appl Physiol. 2011;111(4):1199-1200.
49. Booth FW, Laye MJ, Roberts MD. Lifetime sedentary living accelerates some aspects of secondary aging. J Appl Physiol. 2011;111(5):1497-1504.
50. Charansonney OL. Physical activity and aging: a life-long story. Discovery medicine. 2011;12(64):177-185.
51. Lee IM, Paffenbarger RS, Jr., Hennekens CH. Physical activity, physical fitness and longevity. Aging (Milano). 1997;9(1-2):2-11.
52. Lanza IR, Nair KS. Mitochondrial function as a determinant of life span. Pflugers Archiv : European journal of physiology. 2010;459(2):277-289.
53. Wisloff U, Nilsen TI, Droyvold WB, et al. A single weekly bout of exercise may reduce cardiovascular mortality: how little pain for cardiac gain? ‘The HUNT study, Norway’. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2006;13(5):798-804.
54. Wen CP, Wai JP, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378(9798):1244-1253.
55. Blair SN, Kohl HW, 3rd, Barlow CE, et al. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA : the journal of the American Medical Association. 1995;273(14):1093-1098.
56. Booth FW, Chakravarthy MV, Gordon SE, et al. Waging war on physical inactivity: using modern molecular ammunition against an ancient enemy. J Appl Physiol. 2002;93(1):3-30.
57. Rehn TA, Winett RA, Wisloff U, et al. Increasing physical activity of high intensity to reduce the prevalence of chronic diseases and improve public health. The open cardiovascular medicine journal. 2013;7:1-8.
58. Fries JF. The theory and practice of active aging. Current gerontology and geriatrics research. 2012;2012:420637.
59. Franco OH, de Laet C, Peeters A, et al. Effects of physical activity on life expectancy with cardiovascular disease. Archives of internal medicine. 2005;165(20):2355-2360.
60. Paffenbarger RS, Jr., Hyde RT, Wing AL, et al. Physical activity, all-cause mortality, and longevity of college alumni. The New England journal of medicine. 1986;314(10):605-613.
61. Lee IM, Skerrett PJ. Physical activity and all-cause mortality: what is the dose-response relation? Medicine and science in sports and exercise. 2001;33(6 Suppl):S459-471; discussion S493-454.
62. Katzmarzyk PT, Lee IM. Sedentary behaviour and life expectancy in the USA: a cause-deleted life table analysis. BMJ open. 2012;2(4).
63. Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. American journal of epidemiology. 2008;167(7):875-881.
64. Dogra S, Stathokostas L. Sedentary behavior and physical activity are independent predictors of successful aging in middle-aged and older adults. Journal of aging research. 2012;2012:190654.
65. Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation. 2011;123(24):2870-2891.
66. Bhupathiraju SN, Tucker KL. Coronary heart disease prevention: nutrients, foods, and dietary patterns. Clinica chimica acta; international journal of clinical chemistry. 2011;412(17-18):1493-1514.
67. Hlebowicz J, Drake I, Gullberg B, et al. A high diet quality is associated with lower incidence of cardiovascular events in the malmo diet and cancer cohort. PloS one. 2013;8(8):e71095.
68. Mente A, de Koning L, Shannon HS, et al. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Archives of internal medicine. 2009;169(7):659-669.
69. Estruch R, Ros E, Salas-Salvado J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. The New England journal of medicine. 2013;368(14):1279-1290.
70. Damasceno NR, Sala-Vila A, Cofan M, et al. Mediterranean diet supplemented with nuts reduces waist circumference and shifts lipoprotein subfractions to a less atherogenic pattern in subjects at high cardiovascular risk. Atherosclerosis. 2013;230(2):347-353.
71. Ibarrola-Jurado N, Bullo M, Guasch-Ferre M, et al. Cross-sectional assessment of nut consumption and obesity, metabolic syndrome and other cardiometabolic risk factors: the PREDIMED study. PloS one. 2013;8(2):e57367.
72. Pan A, Sun Q, Manson JE, et al. Walnut consumption is associated with lower risk of type 2 diabetes in women. The Journal of nutrition. 2013;143(4):512-518.
73. McCullough ML, Peterson JJ, Patel R, et al. Flavonoid intake and cardiovascular disease mortality in a prospective cohort of US adults. The American journal of clinical nutrition. 2012;95(2):454-464.
74. Mozaffarian D, Lemaitre RN, King IB, et al. Plasma phospholipid long-chain omega-3 fatty acids and total and cause-specific mortality in older adults: a cohort study. Annals of internal medicine. 2013;158(7):515-525.
75. Tong X, Dong JY, Wu ZW, et al. Dairy consumption and risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. European journal of clinical nutrition. 2011;65(9):1027-1031.
76. Trovato GM. Behavior, nutrition and lifestyle in a comprehensive health and disease paradigm: skills and knowledge for a predictive, preventive and personalized medicine. The EPMA journal. 2012;3(1):8.
77. Knoops KT, de Groot LC, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA : the journal of the American Medical Association. 2004;292(12):1433-1439.
78. Today AN-U. Poll: Living Longer, Living Better. In October 16, (Ed). http://abcnews.go.com/images/Politics/995a1Longevity.pdf 2006.
79. Abrahamson S. Time to return medical schools to their primary purpose: education. Academic medicine : journal of the Association of American Medical Colleges. 1996;71(4):343-347.
80. Frank E, Tong E, Lobelo F, et al. Physical activity levels and counseling practices of U.S. medical students. Medicine and science in sports and exercise. 2008;40(3):413-421.
81. Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their counselling practices. British journal of sports medicine. 2009;43(2):89-92.
82. Moynihan R. Doctors’ education: the invisible influence of drug company sponsorship. BMJ. 2008;336(7641):416-417.
83. Matheson GO, Klugl M, Dvorak J, et al. Responsibility of sport and exercise medicine in preventing and managing chronic disease: applying our knowledge and skill is overdue. British journal of sports medicine. 2011;45(16):1272-1282.
84. Mohler MJ, D’Huyvetter K, Tomasa L, et al. Healthy aging rounds: using healthy-aging mentors to teach medical students about physical activity and social support assessment, interviewing, and prescription. Journal of the American Geriatrics Society. 2010;58(12):2407-2411.
85. Gottlieb LK, Holman HR. What’s preventing more prevention? Barriers to development at academic medical centers. Journal of general internal medicine. 1992;7(6):630-635.
86. Brun D, Hassid S, d’Ivernois JF. [How do physicians evaluate their medical school training. Retrospective survey of 4 groups of medical students 8-11 years after graduation]. Presse Med. 1999;28(21):1121-1127.
87. Pomrehn PR, Davis MV, Chen DW, et al. Prevention for the 21st century: setting the context through undergraduate medical education. Academic medicine : journal of the Association of American Medical Colleges. 2000;75(7 Suppl):S5-13.
88. Fishman JR, Settersten RA, Jr., Flatt MA. In the vanguard of biomedicine? The curious and contradictory case of anti-ageing medicine. Sociology of health & illness. 2010;32(2):197-210.
89. Mykytyn CE. Anti-aging medicine: a patient/practitioner movement to redefine aging. Soc Sci Med. 2006;62(3):643-653.
90. Kones R. Is prevention a fantasy, or the future of medicine? A panoramic view of recent data, status, and direction in cardiovascular prevention. Therapeutic advances in cardiovascular disease. 2011;5(1):61-81.
91. Fries JF, Bruce B, Chakravarty E. Compression of morbidity 1980-2011: a focused review of paradigms and progress. Journal of aging research. 2011;2011:261702.
92. Klatz R. Anti-Aging medicine and why it must be part of your practice. http://www.chiroweb.com/mpacms/dc_ca/article.php?id=52406 2007.
93. Blagosklonny MV. Answering the ultimate question “what is the proximal cause of aging?”. Aging. 2012;4(12):861-877.
94. Vita AJ, Terry RB, Hubert HB, et al. Aging, health risks, and cumulative disability. The New England journal of medicine. 1998;338(15):1035-1041.
95. Hubert HB, Bloch DA, Oehlert JW, et al. Lifestyle habits and compression of morbidity. The journals of gerontology Series A, Biological sciences and medical sciences. 2002;57(6):M347-351.
96. Fries JF. Aging, natural death, and the compression of morbidity. The New England journal of medicine. 1980;303(3):130-135.
97. Kalache A, Aboderin I, Hoskins I. Compression of morbidity and active ageing: key priorities for public health policy in the 21st century. Bulletin of the World Health Organization. 2002;80(3):243-244.
98. Andersen SL, Sebastiani P, Dworkis DA, et al. Health span approximates life span among many supercentenarians: compression of morbidity at the approximate limit of life span. The journals of gerontology Series A, Biological sciences and medical sciences. 2012;67(4):395-405.
99. Willcox BJ, Willcox DC, Ferrucci L. Secrets of healthy aging and longevity from exceptional survivors around the globe: lessons from octogenarians to supercentenarians. The journals of gerontology Series A, Biological sciences and medical sciences. 2008;63(11):1181-1185.
100. Willcox DC, Willcox BJ, Wang NC, et al. Life at the extreme limit: phenotypic characteristics of supercentenarians in Okinawa. The journals of gerontology Series A, Biological sciences and medical sciences. 2008;63(11):1201-1208.
101. Engberg H, Oksuzyan A, Jeune B, et al. Centenarians–a useful model for healthy aging? A 29-year follow-up of hospitalizations among 40,000 Danes born in 1905. Aging cell. 2009;8(3):270-276.
102. Leyk D, Ruther T, Wunderlich M, et al. Physical performance in middle age and old age: good news for our sedentary and aging society. Deutsches Arzteblatt international. 2010;107(46):809-816.
103. Wang BW, Ramey DR, Schettler JD, et al. Postponed development of disability in elderly runners: a 13-year longitudinal study. Archives of internal medicine. 2002;162(20):2285-2294.
104. Hawkins SA, Wiswell RA, Marcell TJ. Exercise and the master athlete–a model of successful aging? The journals of gerontology Series A, Biological sciences and medical sciences. 2003;58(11):1009-1011.
105. Willcox DC, Willcox BJ, Poon LW. Centenarian studies: important contributors to our understanding of the aging process and longevity. Current gerontology and geriatrics research. 2010;2010:484529.
106. Singh AR. Modern Medicine: Towards Prevention, Cure, Well-being and Longevity. Mens sana monographs. 2010;8(1):17-29.
107. Keipes M, Bellucci A, Hansen E. Risk factors and disease prevalence in 3331 personal check-ups performed in preventive medicine between 2006 and 2011. cross-sectional and follow-up study. Bulletin de la Societe des sciences medicales du Grand-Duche de Luxembourg. 2012(2):25-35.